Claims are reviewed for accuracy and full required information, then submitted to clearinghouse for scrubbing quickly after the patient visit. We’ll stay up-to-date with all your payers’ requirements so “clean” claims are submitted and paid the first time.
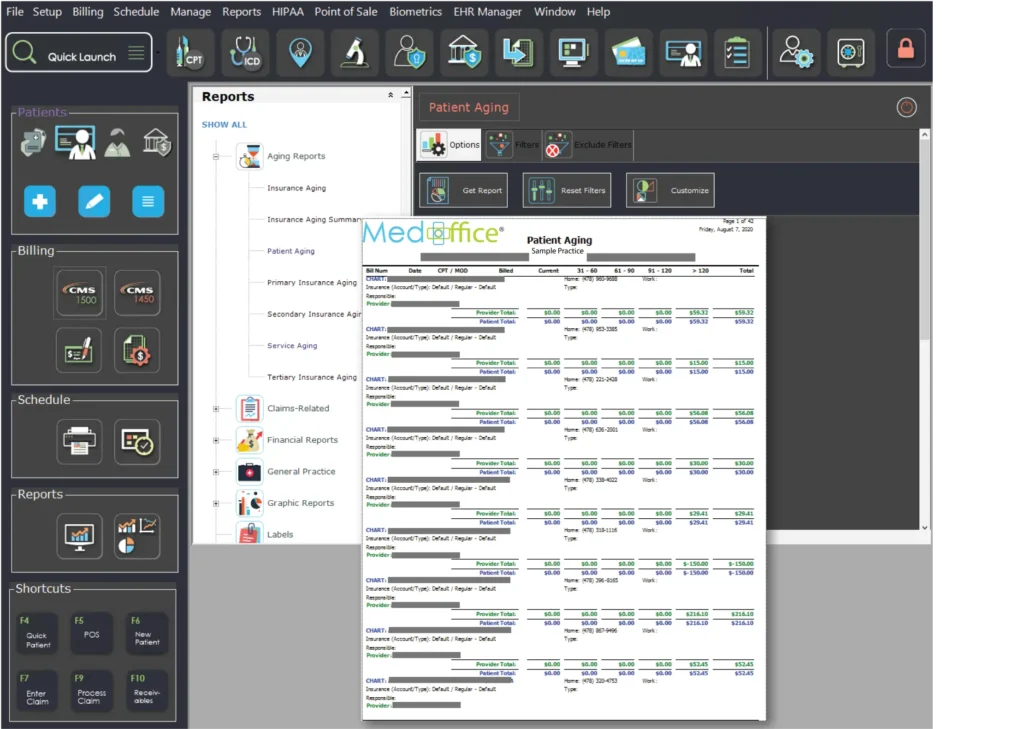
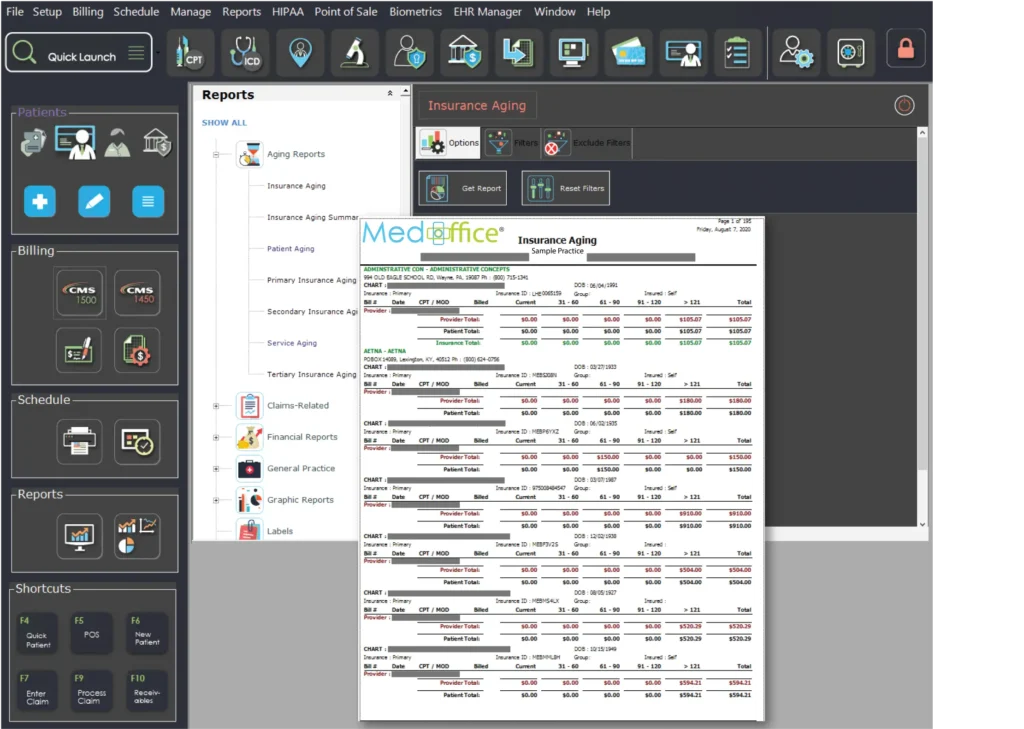
Receivables and claim balances are monitored to identify and address any payment delays. We are diligent with follow up and go after every dollar. Supporting documentation is submitted when necessary.
If a claim is denied, we will investigate and re-submit with the correction or appeal immediately. The practice will be notified and we will work to eliminate future denials. No claims are written off without consent.
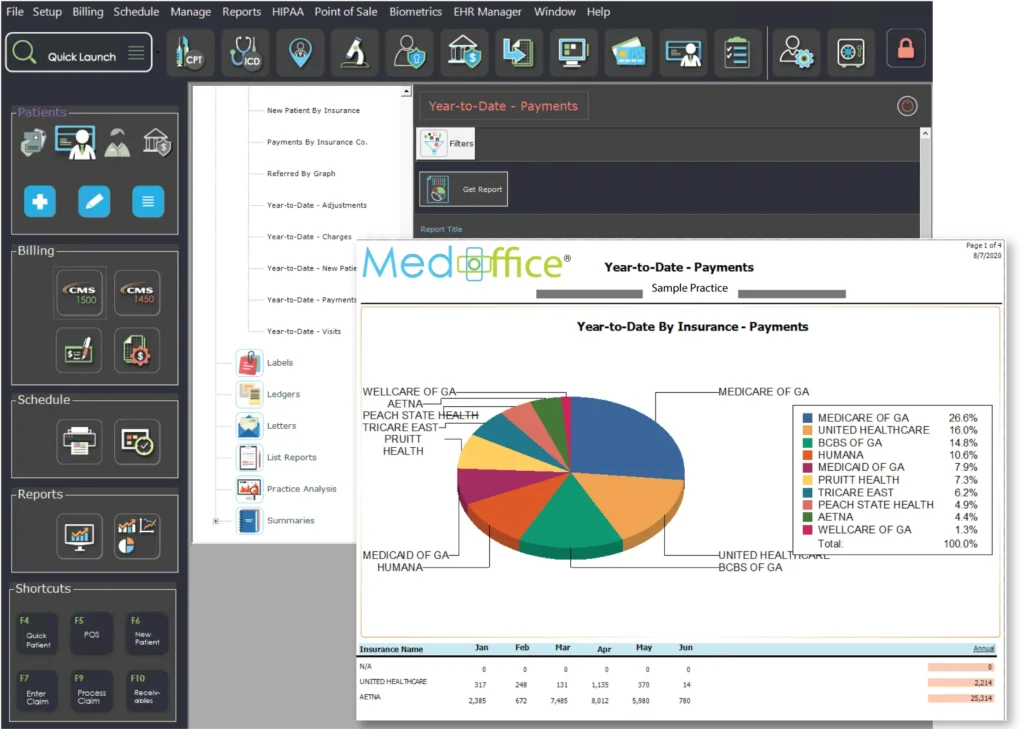
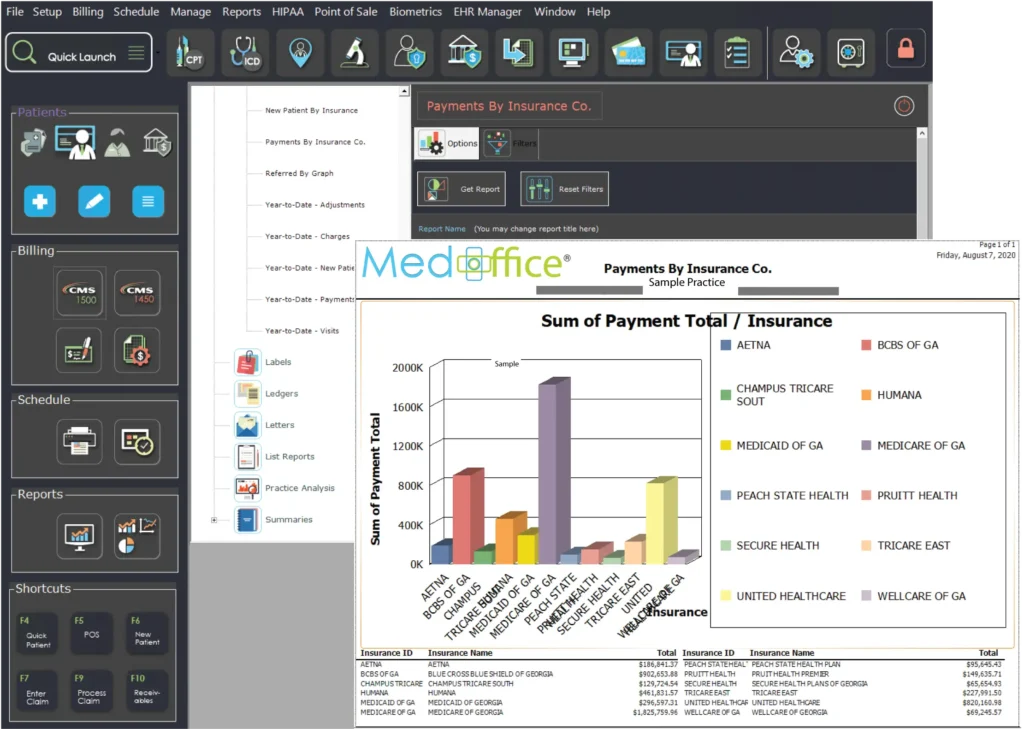
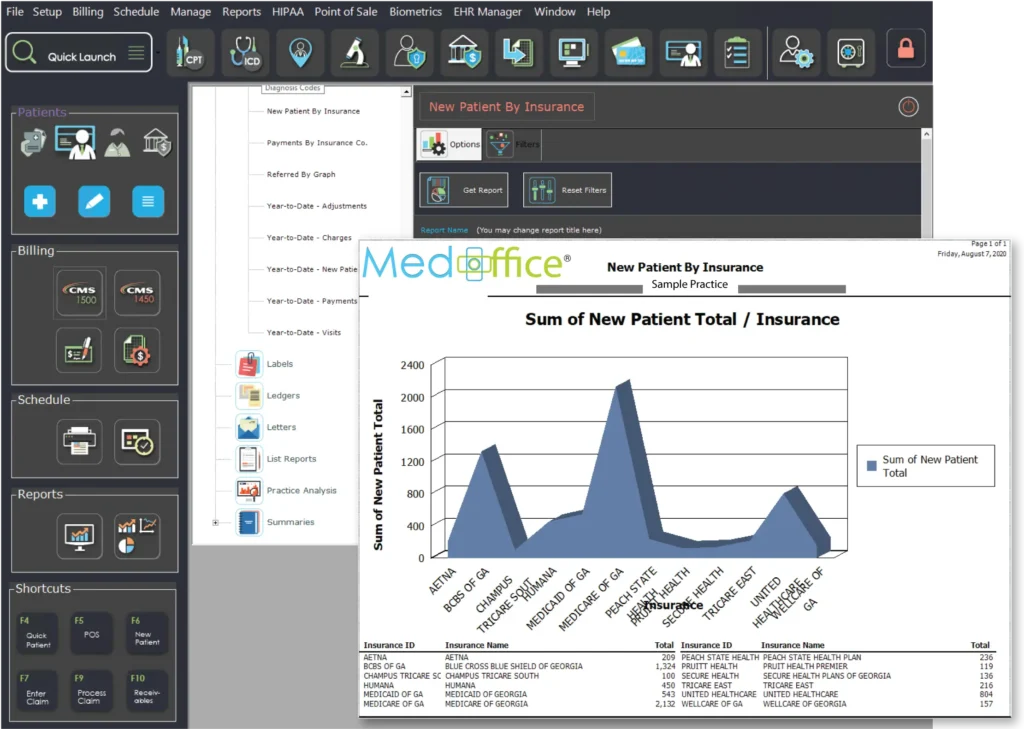
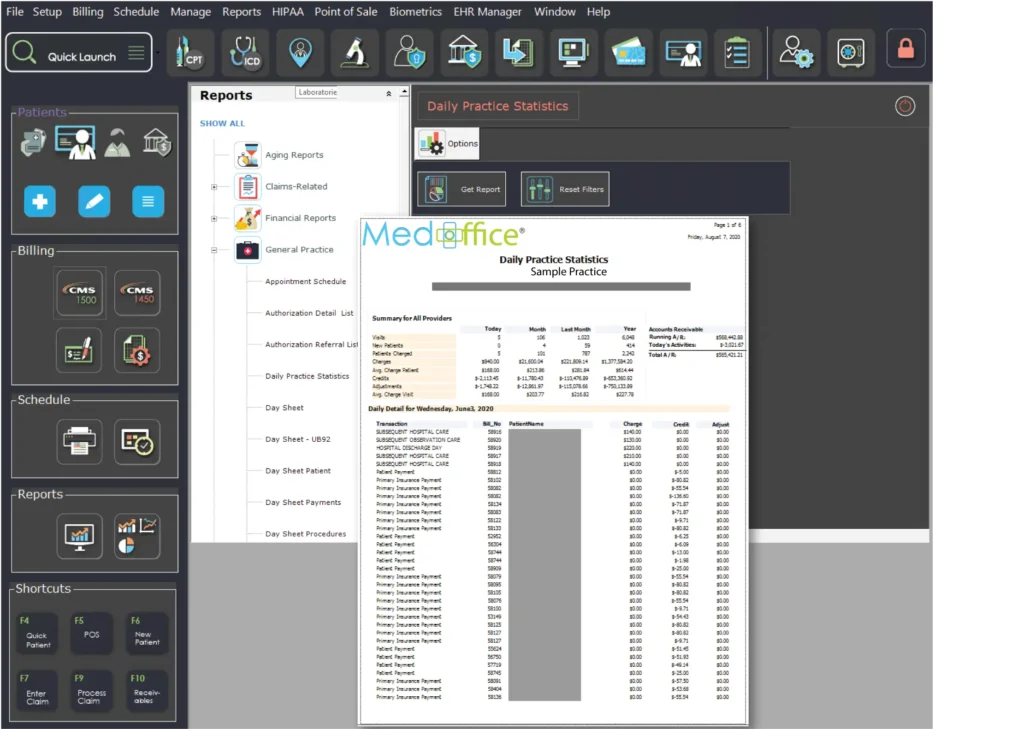
We post ERA’s and EOB’s to maximize accuracy and speed of billing cycle. Our billing software automates the revenue cycle from primary insurance to secondary and then to the patient (when applicable) so no steps are missed.